
Homemade Meals for Busy Families
Mary Beth Lagerborg, co-creator of Once-A-Month-Cooking, discusses the importance of hospitality and how families can prioritize dinner time by cooking a month’s worth of healthy meals in one session.
Rescue 2x the babies from abortion!
Home » Episodes » Focus on the Family Broadcast » A Godly Perspective on End-of-Life Decisions (Part 2 of 2)
Preview:
Dr. Kathryn Butler: I- I think that hospitals have a way of driving us to our knees. Um, of- as patients, as caregivers, as physicians, and really churning up some very profound and cutting spiritual questions that we have very little support for in the hospital environment.
End of Preview
John Fuller: That’s Dr. Kathryn Butler, describing the turmoil that many families experience with loved ones in the ICU. Dr. Butler joins us again today on Focus on the Family. Your host is Focus president and author, Jim Daly, and I’m John Fuller.
Jim Daly: John, last time we began an insightful conversation with Katie on a godly approach to end of life decisions. And I realize that you probably don’t talk about this often, uh, but it’s important. This is a heavy topic, and, uh, a good topic to have, within the family particularly. Today we’re gonna hear additional, you know, painful stories like we did last time. And if you missed it, get the download, uh, the app, and you can listen that way, or get a hold of us and we’ll give you a link or … We’ll get it to you somehow. Um, a highlight of our discussion yesterday was the reminder of the hope we have as believers. Um, we don’t have to have a heavy heart about this transition from this life to the next. That’s the whole point, isn’t it? That we have eternal life in Jesus. And I was so grateful that Katie wove that into the discussion yesterday. She’s an impressive young woman, a doctor, a trauma physician, and, uh, she’s now a homeschooling mom, which I think is probably the most important job. And I was so delighted to, uh, talk with her last time. If you missed part of it, again, get the download. We’re gonna continue the discussion on advanced directives and those things that trauma surgeons see every day.
John: Yeah, and last time, uh, Jim, for those who watch on YouTube, they saw me writing some notes. I do that, uh, during interviews. And- and one of the notes I wrote down was, we touched on advanced medical directives, and I thought, oh, I need to make sure ours are up to date. And then I thought, oh, we have elderly parents. I need to make sure that we know what their wishes are now, before something happens. So really practical, very helpful conversation. More to come today. Uh, let me just say that Dr. Butler has captured so much of her wisdom and insights, uh, in a great book. It’s called Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care. Of course, we have that here at Focus on the Family. Just call 1-800, the letter A, and the word FAMILY or stop by focusonthefamily.com/broadcast for your copy.
Jim: Uh, Katie, last time you mentioned these four core principles, which really is the basis for the book. Can you, uh, refresh us? And those that didn’t hear yesterday’s program, tell us what those four principles are.
Dr. Butler: S- sure. So, a- a biblical approach to end-of-life care focuses on the fact that life is sacred and something that we’re called to protect. And in that setting, in end-of-life scenarios, it prompts us to try to seek after treatments that have the potential to cure, to bring about full recovery. However, also, God ultimately has authority over our life and death, and death is something that will come to all of us, and he can work even through our death for the good of those who love him. And so, while we are called to protect life, and should pursue treatments with the potential for cure, at the end of life, when our measures don’t promise recovery, we should be very careful about foisting treatments that are potentially futile on people. The third is that we’re to have mercy and compassion and love our neighbor as ourselves. And when it comes to the bedside in these scenarios, that means having an awareness of the fact that our treatments can cause suffering, sometimes very marked suffering. And the fourth, which is the most important of all, is that we have hope in Christ that transforms death from something to be feared at all costs to something that through the cross brings us into eternal communion with the Lord.
Jim: Yeah. And those are all great principles-
John: They are.
Jim: … and we covered them, again, in pretty good detail last time. So, get the download. Um, let’s talk today a little bit more about ICU. You mentioned it yesterday. I can’t imagine that environment. You know, I come to work, we have a program, we talk to people, we help people. We do our own form of triage with people who call us that need help. And it’s rewarding. I can’t imagine being a doctor in the ER like you did for ten years, where you have people with tremendous physical issues, broken bones, car accidents, gunshot wounds, all those things going on. The intensity that you experience as a doctor, especially as a Christian doctor, trying to bring healing to people in that moment. Um, describe that ICU environment like that, and the ER really.
Dr. Butler: I- I think that hospitals have a way of driving us to our knees.
Jim: Huh.
Dr. Butler: Um, of- as patients, as caregivers, as physicians, and really churning up some very profound and cutting spiritual questions that we have very little support for in the hospital environment. Um, and- and part of my concern in talking about end-of-life care is because I think that there’s very little support for patients and their families in wrestling through some of these spiritual issues.
Jim: Yeah.
Dr. Butler: Um, in- in one study, looking at terminally ill patients with cancer, talking about what they anticipate, and the questions that they had about the end of life, 85% of them sa- said they had spiritual concerns, but only 1% said they’d been referred to chaplaincy by their doctor.
Jim: Yeah. Hm.
Dr. Butler: You know, very underutilized. Another study showed that, uh, in conferences between family members and doctors about end-of-life care, that 80% of them h- brought up spiritual questions, and the most common response from the doctor was silence.
Jim: Yeah.
Dr. Butler: And rarely a platitude. But- but never coming alongside and digging deeper and engaging. Um, which is concerning because the- the care we receive and the choices we make depend upon our faith and our spiritual concerns. So, it’s an environment that’s ripe with suffering, and I think the gospel and the cross lends meaning to it, because when you know who God is, and when you know what he has done for us in Christ, and that Jesus came and laid down his life for us who are so undeserving, you seem glimmers through of his love, even in the heartache. I- I- in my most recent book that’s coming out, one of those instances that still rests with me so heavily was a gentleman who had been in the ICU for months and months, and what happens when you’re in the ICU for a long period of time is you start to accrue complications, and it gets harder and harder to get better.
Jim: Right.
Dr. Butler: You start to go into wasting, you devour your own muscle tissue, uh, and you then start to stack on infections from the measures we give you. You know? So, every line we put in ca-
Jim: So, it’s all complicating.
Dr. Butler: … risks- right, risks giving you an infection. The longer you’re on the ventilator, the harder it is to get off, because your respiratory muscles atrophy. You know, so over … The longer you’re in the ICU, the harder it is to get out. And he had been in that position and finally after months and months he was at the point where we had nothing more to do for him, and he was actively dying. His wife had been at his side, praying over him, holding his hand, communicating with us for months throughout this, and I’d had so many discussions with her.
Jim: Yeah.
Dr. Butler: Some during when she was appropriately angry at us, some where she was stoic, some when she would be tearful. But I called her on this one particular evening and she knew from the sound of my voice right away that this was different, that he was dying. And so, I said, “Can you please come in?” And she could tell from the tone of my voice. And she took a breath, and she says, “I’m 40 minutes away. How much time do we have?” And this gentleman was bleeding into his lungs. We couldn’t control it. His oxygen levels had gone from the 90s, which is normal, down to the 70%, which is incompatible with life, and his lips were blue. And we were doing what we could with the ventilator but could not get his oxygen levels back up.
Dr. Butler: And I looked at this, and I said, “He’s gonna probably pass in the next 10 minutes.” So, I just said, “Please, just come.” And so, his nurse and his respiratory therapist and I worked just non-stop at his bedside. I had 19 other patients, and I was having my other colleagues take care of them because I couldn’t leave his bedside, he was that sick. And I’m suctioning him and doing- putting a camera down his airways and trying to suction the blood out, and the respiratory therapist is doing what he can. And finally, we just all stood back with our arms at our sides and said, “There’s nothing more we can do.”
Jim: Yeah.
Dr. Butler: And at that point, I- all I could do was pray. And I just said, Lord, please, they’ve been through this ordeal. H- let him hold on until she gets here. You know? Please. Whatever you need to do. If you need to part the cars like the red sea on Commonwealth Avenue, you know?
Jim: Right.
Dr. Butler: Whatever. Please. Let her get here. And I watched the monitor and was stunned because for the next half hour, his heart continued.
Jim: Just kept going.
Dr. Butler: Yeah. With- with oxygen levels that were not compatible with life. He should have arrested right away. And then the moment she comes rushing into the ICU, she’s got her coat zipped up to her chin still, because it was November in Boston … And she rushes to the bedside, she holds his hand, and at that moment, his heart stopped.
Jim: Wow.
Dr. Butler: And so, this was this … We- I would see this often, but I would see it only because the Bible convicts us and shows us about how God is good even in calamity. And it was this horrible situation and yes, I would have wanted him to still live, and I wish we could have done more for him, but what a point of grace that he would answer that prayer and allow them one last handhold.
Jim: Yeah.
Dr. Butler: So, you see terrible suffering, and you use horror, but when you truly lean into scripture and see that God’s steadfast love for us endures forever, then you also see glimmers of his- his love and mercy.
Jim: And what a beautiful illustration of the bigger picture.
Dr. Butler: Yeah.
Jim: Right?
Dr. Butler: Yeah.
Jim: I mean, our human existence is just that, it’s just what’s here.
Dr. Butler: Mm-hmm. Right.
Jim: But the spiritual dimension is so much more.
Dr. Butler: Yep.
Jim: That God would hold on-
Dr. Butler: Exactly.
Jim: … you know and let them have that last moment. And, you know, those heartbreaking situations like the one you just described, um, I’ve heard of stories where some people who are struggling with their health at end of life, believe somehow … They interpret that- that they have sinned against God, that he’s not answering prayer, and I’m sure you’ve seen that as a Christian doctor.
Dr. Butler: Yeah.
Jim: How do you- how do you counsel that person-
Dr. Butler: Oh.
Jim: … that’s really heaping on the guilt in the midst of their dying?
Dr. Butler: Yeah. I- I had one mother of a teenager girl for whom I cared, and she had- had just an awful, awful course. She had been in a car accident, and we got her through all the injuries, but she had horrible complications from a feeding tube that we placed. Um, and basically had- her abdomen was locked in with an infection that we never got a handle on. And after three months in the ICU, um, she very clearly was dying, and I had a conversation with her mom, and her mom broke down and said, “Do you think God’s punishing me because I don’t go to church anymore?”
Jim: Oh, wow.
Dr. Butler: “Do you think that’s why she’s dying?” So just like you said, the kind of grief that you can bare, and the guilt … But I think the Bible points us in another direction, that we don’t know always why we suffer, or why awful things happen, but we see so many examples throughout the Bible of God affecting good, that we can’t comprehend, even through our suffering. I think of John 11, when Lazarus is dying and Jesus receives word, and our expectation from the outside would be the only good thing would be for Jesus to go and heal him, right?
Jim: Sure.
Dr. Butler: But he delays, and he tells his disciples, “I’m delaying so that God’s glory might be shown to you.” And he arrives and Lazarus has died in his delay, and Mary and Martha say, “If you’d been here, he would lived.” And there was that- that kind of grief … Why- why weren’t you here? And then he raises Lazarus from the dead in the company of all these mourners who are gathered who can see God’s glory in Christ. Or I think of Genesis 50, verse 20, where Joseph h- was … You know, thrown into a well and sold into slavery, and endured all this suffering at the hand of his brothers, but when he finally meets them afterwards, he says, “You meant this for evil, but God meant it for good. The suffering I endured meant- he meant for good, to save many lives.” Because then he was in Egypt, and he was able to save the nation of Israel by providing food for them.
Jim: Right.
Dr. Butler: Do you know- so you see all of these ways, and the most beautiful manifestation of that is the cross, where God worked through suffering, he worked through the suffering of his son to bring about the greatest gift he’s given to all of mankind. You know, and so what you see is that we might not know the answer for suffering, but we do see that, like from Romans 8:28, he works through all things for the good of those who love him, in even the bad moments. And because something bad has happened doesn’t mean that you’ve done something to earn that punishment explicitly.
Jim: It’s such an encouragement for people struggling. And you know, you think of a mother’s heart-
Dr. Butler: Yeah.
Jim: … and feeling that guilt that my son is dying because of something I did or did not do.
Dr. Butler: Right.
Jim: Um, that doesn’t feel like the heart of God.
Dr. Butler: Mm-hmm.
Jim: It really doesn’t. I think God is for us in hardship, and he wants, you know, what’s best for us. And we’ll always do those things that- that keeps our best interests in mind, even in the suffering.
Dr. Butler: Right.
Jim: And that’s key.
John: Well, this is Focus on the Family, and, uh, your host is Jim Daly, our guest is Dr. Kathryn Butler, and, uh, we are so glad to have this conversation. It is full of scripture and really thoughtful things that we have to consider. Um, Dr. Butler’s book is Between Life and Death: A Gospel-centered Guide to End-of-Life Medical Care. Uh, you can get part one of this conversation, you can get the book, um, you can get other resources, all of that and more at focusonthefamily.com/broadcast.
Jim: Katie, we’re in the last quarter of our two days together, fourth quarter now.
Dr. Butler: (Laughs).
Jim: So, let’s- let’s talk about physician-assisted suicide. We referenced it … Um, I think right now it’s legal in seven states. There’s probably two or three more states that are considering it. So …
Dr. Butler: It’s actually legal in 11 now.
Jim: 11 now?
Dr. Butler: Yeah. Yeah.
Jim: So already it’s moved to 11.
Dr. Butler: Mm-hmm.
Jim: So, in that context, um, what … As a physician, what is your attitude when it comes … And as a Christian, more importantly, what’s your attitude with physician-assisted suicide? Given even some Christians can rationalize this-
Dr. Butler: Mm-hmm.
Jim: … that this is humane, it’s the right thing to do because we’re prolonging life beyond what they would normally live.
Dr. Butler: Right.
Jim: So, this is actually a good thing. Speak to that whole issue.
Dr. Butler: Yeah. We need to be really careful, and- and I- I think it’s unfortunate that physician-assisted suicide is now reaching more widespread approval, because I think people can then misconstrue what we’re talking about, in terms of limiting harmful treatments, right, with …
Jim: Right. When a person is actively dying.
Dr. Butler: When a person is actively dying, right?
Jim: Mm-hmm.
Dr. Butler: With physician-assisted suicide, which is actively ending someone’s life, okay. They’re very different, but I- I worry that in the terminology that’s used, people can misconstrue them. And I- actually I understand the compassion that people have and the stance that people can have looking at this and saying, “Oh, isn’t this a way to love other people and be- show them dignity?” And I, of all people, had a reason, a personal reason, to actually advocate for PAS. I’m gonna say right now, I don’t. But I had a- a family member who suffered from, um, amyotrophic lateral sclerosis, Lou-Gehrig’s disease.
Jim: Right.
Dr. Butler: And so, he was very fiercely independent and proud and aloof, and saw suddenly his ability to eat, speak, feed himself, clean himself, gone. And in the setting of the- the turmoil that thrust him into, he took his own life. Before he took his own life, he wrote a series of letters. One to his wife, uh, encouraging her. One telling her to call 911, because he had planned it ahead of time and knew she would find him. And the last, he wrote a note and said, “Support Kevorkian.” And Kevorkian was the doctor from … I think it was 20 years ago.
Jim: Doctor Death.
Dr. Butler: Who was- yes, he was an advocate for euthanasia, which is a- a close cousin of physician-assisted suicide. So that was very present in my mind when I went to medical school. And I would see the kind of suffering we would inflict, and- and sympathize, and- and wonder. But as I would walk through the hallways and see my patients, like, I could never give them pills to help them end their life. How- how could I do that? You know, and so in- inwardly, even before I was a Christian, even though I had a reason personally to advocate for it, I knew it was wrong. And when you look at what the Bible teaches us, you know, there is a difference between refusing treatment that’s going to cause suffering and not health, and actively ending your life with medication. Physician-assisted suicide is that. It’s the doctor gives you medication, usually a high dose of a barbiturate, that you take and that is what ends your life. Not the underlying illness that’s troubling you. Um, euthanasia, which is now legal in Canada, is actually giving a lethal injection. The physician actually gives a lethal injection to someone to end their life. Very different, and that’s actively taking life, and brings us right back to Mt. Sinai, with do not murder. There- there is a very clear distinction between the two. And it’s important for us to be clear on this, because the- the movement in favor of physician-assisted suicide likes to soften terms. So, there was a Gallup poll done about 10 years ago in which they phrased, “Do you think it’s okay for a doctor to help someone end their life without suffering?” And 64% said yes.
Jim: Right. It sounds like a good thing.
Dr. Butler: When you change … Right. When you change the term to suicide-
Jim: Yeah.
Dr. Butler: … the approval went down to 15%. People know it’s wrong, but when you monkey with the language suddenly it sounds more acceptable. And that’s what has happened, is there is an active debate that physician-assisted suicide, which is the appropriate terminology, should be changed to medical aid in dying.
John: Mm-hmm.
Dr. Butler: So, it’s just important for people to be aware. This is not the same as transitioning to comfort measures or withdrawing from life support. It’s something active. It’s the active taking of a life.
Jim: Right. It’s so important. And I hope people hear that clarification. And again, there’s more in your book, and- that they can read. Um, let’s move to those, uh, directives that, uh, you’ve mentioned throughout yesterday and today. Um, let’s give a- another quick recap of, uh, the advance directives, and then what is some of the best examples that you’ve seen that really have helped you as a doctor, and the hospital, uh, where families have thought this through and really- really, uh, given you the direction you need?
Dr. Butler: Yeah. You know, so nobody likes to talk about these issues. You can … There’s no quicker way to shut up conversation during dinner than to bring up death. Nobody wants to-
Jim: (Laughs). Yeah, right, it’s not … It’s not party talk.
Dr. Butler: … (Laughs). Nobody wants to talk about it. And- and it- the questions make us uncomfortable; you know. But the problem is that when we don’t talk about it with our families, we risk straddling them and abandoning them to- in some really hard situations. So, what do I mean by that? 75% of us will not be able to vouch for ourselves at the end of life.
Jim: Wow.
Dr. Butler: Either because the interventions we’re on will rob us- rob us of a voice, or we’re going to be too sick to actually speak our wishes. However, only one in four people in America has an advanced directive on file guiding loved ones on what they should do.
Jim: So, it’s actually the a- absolute inverse, right?
Dr. Butler: Yes. Yes. So- so most of us will not be able to speak for ourselves and will rely upon our- our loved ones’ next of kin to make decisions on our behalf, but only about one fourth of us has actually given them instructions to do so. So advanced directives are in- are to try to guide our loved ones when we can’t speak for ourselves, and also to ensure that our own wishes are respected. And they come in a number of flavors. The first thing is appointing a healthcare proxy, or a durable healthcare power of attorney, which is someone that you appoint to advocate on your behalf and make decisions when you can’t speak for yourself. And it’s very important to do this because, uh, number one, you want to make sure that you have discussions with that family member and that they are comfortable making decisions for you-
Jim: Right.
Dr. Butler: … and that they know your wishes. Um, and also because if you have one that you specifically designated, it can alleviate some of the turmoil between family members when disagreements come up. So, if you’ve had a discussion with your- your son or daughter, and another son or daughter disagrees with what’s decided upon, that person that you’ve designated can at least say, “I know this is what mom or dad would want. We talked about it.”
Jim: Yeah.
Dr. Butler: So, it- it helps to equip them.
Jim: You have a powerful story about a woman who was prepared to make decisions for her sister, and I think you expressed that as one of the better examples of how to do this. What happened?
Dr. Butler: Yeah. So, I had to, um, help out a colleague in the operating room who was in crisis. Um, he was caring for a woman who had a large tumor in her pelvis, and in trying to excise it there was a network of blood vessels adhered to it, and they all tore. And so, she spilled her blood volume into her pelvis in the span of a few minutes. So, he called for help, I arrived, and the anesthesiologist was doing CPR, and we worked together and packed the pelvis and gave several units … Not several- several liters of blood. Um, stabilized her enough, sent her to interventional radiology to see if we could stop the bleeding with catheters. Could not do it. Came back to the operating room, packed again. Brought her up to the intensive care unit where I had to, a third time, go in and try to stop the bleeding. And it had been hours and hours of us trying to- to save her, and it was very clear that we were losing, and we were not going to be able to. And I had talked to her sister throughout this, and she understood and was very nervous, and asked the appropriate questions. But I called and she could hear from the tone of my voice that we were at the end. And so, I said, “Please come in now.” And when I went to see her in the waiting room, she looked like her sister, she looked like my patient.
Jim: Mm-hmm.
Dr. Butler: And she’s sitting there jangling her keys, and for … I had this one eerie moment where I- my mind did a flip on me, and I thought maybe she’s okay. (Laughs). Um, but sat down and was trembling, because we’d been working so hard and it’s hard to admit that no, we can’t- we can’t save her. And she stopped me mid-sentence and said, “My sister wouldn’t want any of what you’re doing right now.” And I was so surprised by the conviction with which she said it and the calm with which she said it. And she had tears in her eyes, and she said, “I- I- I don’t want to let my sister go, I don’t want to lose her, but we talked about this so many times. We watched my mom die in the ICU and it was horrible, and we so clearly talked together about what would be okay for us, and what wouldn’t. And she wouldn’t want anything of what you’re doing right now. You know, she has faith in God and just let her go to be with God. Can I see her before you let her go?” And so, she went and she spent her last moments with her sister. But she said, she’s like, you know, “I don’t want to lose her, but I at least- I know what she wanted.”
Jim: Yeah.
Dr. Butler: And so, it just shows that the power … If you have these discussions, as difficult as they are, it can equip our loved ones in moments that are going to be horrendous for them, that are gonna be sad, that are going to cause them grief and fear, but at least they have the solace to say, “I know what my loved one would have wanted, and I have respected that.”
Jim: Yeah.
Dr. Butler: And it can bring peace in a situation that’s otherwise horrible.
John: Mm-hmm.
Jim: Katie, this has been so good. I mean, we have flown by two days. And I- I hope people have appreciated, maybe not enjoyed, but appreciated, the discussion. I- I appreciate your courage in writing it as a physician. Let me, uh, let me end with this question. Because I’m so impressed by who you are, it brings me to tears. I mean, you just are such a phenomenal individual, and, uh, you know, becoming a physician and the way you’ve applied it, and the way you work scripture into everything. It’s really refreshing that, um, your science has not voided your faith. So let me give you the last word to talk to people about that intersection of faith.
Dr. Butler: Yeah. I- I would just say that these situations are so harrowing, and they can bring us to just the deepest anguish. And afterwards, whether or not things have gone smoothly, when you make a decision for a loved one, you can be struggling afterwards with questions of why, did I do the right thing, and guilt. And I would just say, in all things just turn to Christ, because he’s the founder and perfecter of our faith, and he reminds us, even in these horrible situations when we’re dealing with death and illness, that although our hearts and our flesh may fail, he’s the strength of our heart and our portion forever. And no matter what assails us, we have forgiveness and hope in him.
Jim: That is well said. Uh, Katie Butler, Dr. Butler, thank you for being with us.
Dr. Butler: Thank you.
Jim: This has been so informative. Thank you.
Dr. Butler: Thank you.
Jim: And for the listeners and the viewers, uh, this is the kind of resource you need on your shelf, and you need to be looking at it and reading it together as a couple and talking about what it is you need to plan for for those end-of-life issues. Or maybe it’s something you need to help, again, with your grandparents, or your parents. They’re aging and you need to make decisions, and maybe sooner rather than later.
Jim: And as we often do, you know, we want to make this available to you. So, if you can, make a gift of any amount. Uh, be a part of the ministry so we can help families who can’t get this resource. Uh, but make a gift of any amount and we’ll send you Katie’s, uh, book, as our way of saying thank you. If you can’t afford it, we often say this with marriage advice and parenting tools, just get in touch with us. Uh, we’ll trust others will cover the cost of that. If you need this resource and you can’t help us in ministry, we want to minister to you. So, get in touch with us and we’ll get it in your hands.
John: Yeah. And, uh, Dr. Butler’s book, once again, is called Between Life and Death: A Gospel-centered Guide to End-of-Life Medical Care. We’d love to get a copy to you. And, uh, one more thing that we say often here, Jim, is that we have caring Christian counselors. Uh, we’ve talked through some tough stuff here, and if you need to talk with someone about your circumstances, uh, schedule a time with one of those counselors. Or get the book and donate as you can when you call 800, the letter A, and the word FAMILY. Next time, Shaunti Feldhahn offers encouragement for your marriage based on lessons she’s learned after interviewing hundreds of couples who are truly happy in their relationship.
Preview:
Shaunti Feldhahn: There is a principle here that is incredibly important about looking for the bright spots and seeing what those role models, the people who have the happiest marriages have to teach us.
End of Preview
John: On behalf of Jim Daly and the entire team, thanks for joining us today for Focus on the Family. I’m John Fuller, inviting you back as we once again help you and your family thrive in Christ.

Dr. Kathryn Butler trained in surgery and critical care at Massachusetts General Hospital and Harvard Medical School, where she then joined the faculty. Dr. Butler left clinical practice in 2016 to homeschool her children and now writes regularly for desiringGod.org and the Gospel Coalition on topics such as faith, medicine, and shepherding kids in the gospel. She is the author of Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care (Crossway, 2019), and Glimmers of Grace: A Doctor’s Reflections on Faith, Suffering, and the Goodness of God (Crossway, 2021). She lives with her husband and two kids north of Boston.
Receive Dr. Kathryn Butler's book Between Life and Death for your donation of any amount!
Visit our online store and purchase a CD of today's program for yourself or to share with a friend.

Focus on the Family's staff of licensed, professional counselors can help you bring healing and restoration to your family with Christian perspectives you can trust.
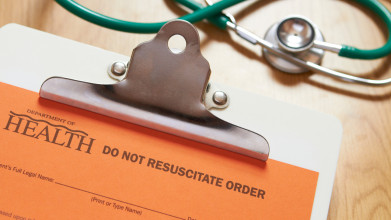
End-of-life medical care is complicated and sometimes murky, often requiring quick decisions on matters of life and death. Having a plan in place can make all the difference.

Can you tell me how to make sure that my elderly father's medical wishes will be respected? He's in ill health, and he has often said that he doesn't want any heroic measures taken to prolong his life.

Knowing Bible verses about death and pain, as well as how we should respond to each, can help us better serve those facing end of life hardships.

Here are some top pro-life movies and books that encourage conversation about adoption, preborn, special needs and elderly.
Joni Eareckson Tada examines the dangerous ramifications of the "right-to-die movement" and "mercy killing," and encourages listeners to consider how we can all demonstrate love and compassion to those with disabilities and end-of-life challenges.
Joni Eareckson Tada describes how the weak and vulnerable in our society are being stripped of value and dignity, and urges Christians to stand against today's culture of death by fighting against abortion, assisted suicide, and euthanasia.

Mary Beth Lagerborg, co-creator of Once-A-Month-Cooking, discusses the importance of hospitality and how families can prioritize dinner time by cooking a month’s worth of healthy meals in one session.

Scott Klusendorf, President of The Life Training Institute and Robyn Chambers, Vice President of Advocacy for Children at Focus on the Family, share strategies and encouragement in the pro-life movement. They offer compassion for abortion-minded women and speak up for pre-born babies. (Part 2 of 2)

Scott Klusendorf, President of The Life Training Institute and Robyn Chambers, Vice President of Advocacy for Children at Focus on the Family, share strategies and encouragement in the pro-life movement. They offer compassion for abortion-minded women and speak up for pre-born babies. (Part 1 of 2)

Larnelle Harris shares stories about how God redeemed the dysfunctional past of his parents, the many African-American teachers who sacrificed their time and energy to give young men like himself a better future, and how his faithfulness to godly principles gave him greater opportunities and career success than anything else.

Amy Carroll shares how her perfectionism led to her being discontent in her marriage for over a decade, how she learned to find value in who Christ is, not in what she does, and practical ways everyone can accept the messiness of marriage and of life.

Jonathan McKee offers parents practical advice and encouragement in a discussion based on his book If I Had a Parenting Do Over: 7 Vital Changes I’d Make.